Silicone oil (SO) may be used in complex retinal detachment surgery, but management of SO in patients with aphakia and iris loss or traumatic mydriasis is challenging, because SO can migrate into the anterior chamber and cause keratopathy, elevated intraocular pressure and a suboptimal oil fill.
Ronald Gentile, MD, and Dean Eliott, MD, described placement of SO retention sutures in such cases, which provide an artificial barrier to decrease risks associated with a unicameral eye.1 Others have described variations of this technique, and a recent series confirmed efficacy in prevention of SO-cornea touch.2
Step-by-Step Guide
Here, John D. Pitcher III, MD, provides a step-by-step guide with accompanying video to show how to successfully employ this technique.
He has made some slight modifications to avoid compromising the visual axis and to reduce the number of necessary suture passes (View the online video at: bit.ly/RS_VideoPearl_001). Here are the key steps:
1. Perform a conjunctival peritomy, which is required to bury the prolene suture ends.
2. Perform retinal detachment repair as indicated.
3. With the eye under fluid and prior to performing the final fluid-air exchange, pass a 10-0 prolene suture with a 16-mm STC-6 straight needle (Ethicon, Somerville, N.J.) behind the iris starting 1 mm posterior to the limbus, just off center from the visual axis.
4. A 27-gauge needle can be bent at the hub and then inserted, bevel up, on the horizontally opposite side of the eye, also 1 mm posterior to the limbus and off center from the visual axis.
 |
5. “Dock” the STC-6 needle in the lumen of the 27-gauge needle and then slowly pull both simultaneously out of the eye.
6. Using the same needle and suture, repeat steps 3 through 5 going back in the other horizontal direction, parallel to the initial pass, approximately 2 to 3 mm away from the central visual axis.
7. Cut off the needle and tie the two ends of the prolene suture in a 3-1-1-1 knot at a moderate tension. Trim residual suture ends.
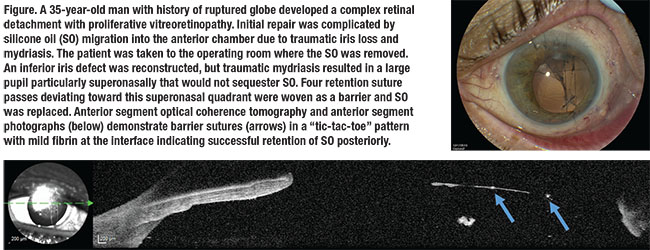
8. Repeat steps 3 through 7 in the vertical direction off center from the visual axis, perpendicular to the initial horizontal sutures. The sutures should be “woven” between the first two, which will bring all four sutures into a single plane, strengthening the surface tension effect (Figure). The result is a “tic-tac-toe” grid barrier, which should deviate toward the area of sectoral iris loss or traumatic mydriasis.
9. Perform air-fluid exchange and SO injection as usual, taking care to avoid filling oil past the level of the sutures.
10. Close sclerotomies and peritomy with an absorbable suture, ensuring that the conjunctiva covers the prolene sutures.
11. Face-down positioning for the first night can help ensure SO remains posterior.
For cases of sectoral iris loss or traumatic mydriasis, Dr. Pitcher has shown that just four passes with placement deviated toward the area of sectoral loss to spare the visual axis can successfully sequester SO posteriorly. Larger areas of iris loss may require more sutures but the concept remains the same. Techniques such as this to deal with complex situations are important to tilt the odds in your favor for surgical success. RS
Dr. Hahn is an associate at New Jersey Retina in Teaneck. Dr. Pitcher is a partner at Eye Associates of New Mexico and assistant professor of ophthalmology at the University of New Mexico, Albuquerque.
REFERENCES
1. Gentile RC, Eliott D. Silicone oil retention sutures in aphakic eyes with iris loss. Arch Ophthalmol. 2010;128:1596-1599.
2. Yuksel K, Pekel G, Alagoz N, Alagoz C, Baz O, Yazc AT. Silicone oil barrier sutures in aphakic eyes with iris defects. Retina. 2016;36:1222-1226.




