 |
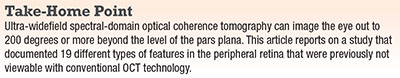 |
This imaging has allowed us to see retinal tufts with great detail and traction, the ora serrata pearl and areas of peripheral cystoid degeneration—areas that have not been imaged with SD-OCT in the past.
 |
| Figure 1. Ultra-widefield pseudocolor image (A) of the right eye demonstrates a retinal tuft, with a high-magnification view (B). Near-infrared reflectance image (C) of a retinal tuft. Spectral-domain optical coherence tomography (D) demonstrates concave vitreous adhesion at the retinal interface of the retinal tuft, while the underlying retinal layers appear normal. |
Here, I will review the types of pathology and features that one can find in the peripheral retina, focusing on three different types of retinal pathology—retinal hole, typical cystoid degeneration and typical degenerative senile retinoschisis—and discuss the significance of our findings.
Our UWF Technique
Our team of investigators used a 30-degree, off-the-shelf lens that comes with the Heidelberg Spectralis SD-OCT device. This study involved an experienced retinal photographer operating a single commercially available SD-OCT device (Heidelberg). This approach registered near-infrared scanning laser ophthalmoscopy images and SD OCT of these entities to UWF color photographs.
Having a skilled retinal photographer is integral in obtaining quality images of the outer retina. Image capture requires significant interplay between photographer and patient, and the process can take five to seven minutes with very compliant patient and skilled photographer. Montaging the images can take 15 to 20 minutes.
To maximize dilation in patients, we administered three sets of standard drops of phenylephrine and tropicamide, and we used an approach similar to what our group previously developed for viewing the seven standard fields for diabetic retinopathy.4
This approach enabled us to direct, or steer, the OCT laser head out to the periphery and obtain high-quality, reproducible SD-OCT images of peripheral retina findings and register the near-infrared reflective images to their Optos 200-degree UWF images. We also used this approach to obtain a continuous, near 200-degree SD-OCT montage from one side of the retinal periphery to the other.
 |
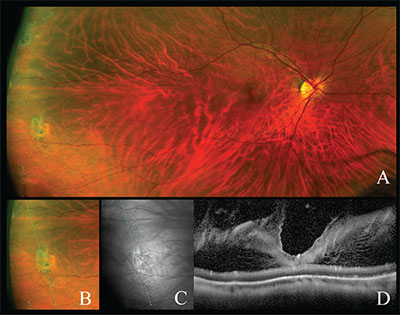
| Figure 2. Ultra-widefield pseudocolor image (A) of the right eye demonstrates an operculated retinal hole. Near-infrared reflectance image (B) of a retinal hole. SD-OCT (C) demonstrates an open retinal hole with a free-floating operculum. Subretinal fluid can be seen at the base of the open the retinal hole. |
When talking about OCT, “widefield” typically means obtaining an SD-OCT image with a 50-degree field of view. UWF, on the other hand, describes capturing a 200-degree field of view in a single image.5-8 In evaluating the retinal periphery, retina specialists have relied upon en-face UWF-based fundus fluorescein angiography and autofluorescence, mostly for imaging vascular diseases. However, this modality does not provide cross-sectional imaging.
Features In The Periphery
Using UWF SD-OCT in the 68 study patients, we were able to identify the following features in the peripheral retina.
Retinal hole. UWF SD-OCT identified 17 retinal holes, all of which revealed subretinal fluid within the hole and the operculum, either attached, partially attached or completely detached (Figure 2). In the retinal holes with a partially attached operculum, we could see vitreous hyper-reflectivity attached to the inner retina, but no such adhesions were visible in adjacent cross sections.
In the retina surrounding the hole, we visualized variable regions of cystoid degeneration with hyper-reflectivity of the subretinal space. When we examined the configuration of the retinal holes more closely, we identified two distinct shapes characteristic of pathology: a V-shape was consistently characteristic of an attached or partially attached operculum; whereas a flat shape was typical of no attached vitreous hyper-reflectivity or subretinal fluid.
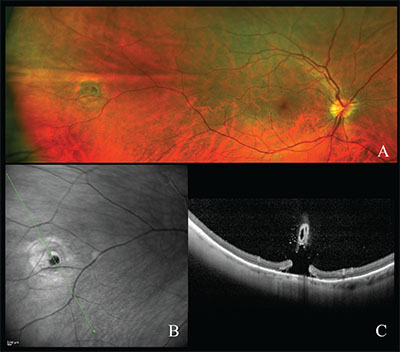
Typical cystoid degeneration. UWF color and near-infrared scanning laser ophthalmoscopy and peripheral SD-OCT provided imaging of typical cystoid degeneration (TCD) in six eyes (Figure 3, page 32). On SD-OCT, hyporeflective cystoid cavities and columns created a saw-tooth pattern that defined the area of TCD. Many of these cavities and columns spanned the entire thickness of the neural retina.
The pars plana epithelium secretes the mucopolysaccharide of the vitreous, and, when imaged, the condensed cortical vitreous appears as a moderately reflective layer above the pars plana and peripheral retina structures. We could also see the ora serrata pearl, which has not been previously imaged. At the apex of the raised surface of the ora serrata pearl, we could also see vitreous adhesion to the inner retina.
 |
| Figure 3. Ultra-widefield pseudocolor image (A) of the right eye demonstrates a peripheral cystoid degeneration, with high-magnification view (B) and a near-Infrared reflectance image (C) of the same. SD-OCT of peripheral cystoid degeneration (D) demonstrates a “saw-tooth” schisis-like separation of the retinal layers. The retinal layers are not distinguishable by their usual laminar orientation. The underlying retinal pigment epithelium appears irregular and the overlying vitreous (formed) is distinct and attached to the inner retina. |
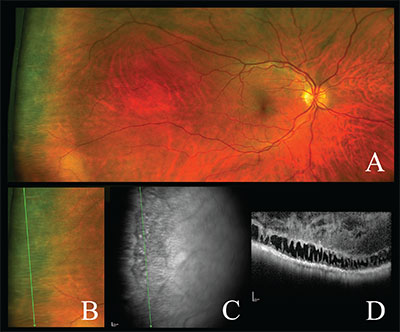
Retinoschisis. We created a continuous UFW montage of an eye with typical degenerative senile retinoschisis, giving us coverage of high-resolution retinal and choroidal features in a single 200-degree image that was not available previously. This involved serial SD-OCTs from periphery to periphery, through the fovea and optic nerve and to the retinoschisis. The montaged image showed schisis of the inner nuclear and outer plexiform layers of the retina posteriorly in the temporal macula that extended into the periphery. The degree of intraretinal splitting widened progressively from the posterior to anterior retina. We also used peripheral SD-OCT to analyze an inferotemporal portion of the retina, revealing schitic splitting along the inner nuclear and outer plexiform layers.
The Potential of UWF SD-OCT
We have shown that UWF SD-OCT is a reproducible technique that can achieve high-quality images with a high level of retinal anatomy and vitreous detail, and in many cases great choroidal detail. The ability to assemble montaged images can provide a “bird’s-eye” view of the retinal periphery. This may give us a greater understanding of the association between pathology in the retinal periphery and the macula.
What’s more, comparing dynamic, cross-sectional images of the retinal periphery over time could improve our understanding of not only cystic retinal tufts, lattice degeneration, retinal holes and retinoschisis with inner and outer layer holes, but even tumors, meridional folds and previously treated or spontaneously scarred retinal tears. Furthermore, SD-OCT with UWF color imaging can allow us to visualize changes in subretinal fluid over time, improving our ability to study the course of these entities and estimate the risk of these findings progressing toward vision impairment.
UWF SD-OCT also has great potential for use in telemedicine. This approach can improve the ability of retina specialists to treat and manage peripheral retinal pathologies via telemedicine in underserved areas. We expect to see a prototype of UWF SD-OCT in the next two years. RS
REFERENCES
1. Diabetic Retinopathy Clinical Research Network (DRCRnet) Public Web Site. Protocol:Peripheral Diabetic Retinopathy (DR) Lesions on Ultrawide-field Fundus Images and Risk of DR Worsening Over Time. http://drcrnet.jaeb.org/Studies.aspx?RecID=239. Accessed August 30, 2019.
2. Choudhry N, Golding J, Manry MW, Rao RC. Ultra-widefield steering-based spectral-domain optical coherence tomography imaging of the retinal periphery. Ophthalmology. 2016. In press.
3. Choudhry N. Ultra-widefield steering-based SD-OCT imaging of the retinal periphery. Paper presented at: 34th annual meeting of the American Society of Retina Specialists. August 11, 2016. San Francisco, CA.
4. Early Treatment Diabetic Retinopathy Study Research Group Grading diabetic retinopathy from stereoscopic color fundus photographs: an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology. 1991;98:786–806.
5. Mori K, Kanno J, Gehlbach PL, Yoneya S. Montage images of spectral-domain optical coherence tomography in eyes with idiopathic macular holes. Ophthalmology. 2012;119:2600–2608.
6. Kothari A, Narendran V, Saravanan VR. In vivo sectional imaging of the retinal periphery using conventional optical coherence tomography systems. Indian J Ophthalmol. 2012;60:235–239.
7. Gregori NZ, Lam BL, Gregori G, et al. Wide-field spectral domain optical coherence tomography in patients and carriers of X-linked retinoschisis. Ophthalmology. 2013;120:169–174.
8. Soliman AZ, Silva PS, Aiello LP, Sun JK. Ultra-widefield retinal imaging in detection, classification, and management of diabetic retinopathy. Semin Ophthalmol. 2012;27:221–227.



