The severity scale from the Age Related Eye Disease Study (AREDS) predicts an increased risk of MNV in eyes with dry AMD when the fellow eye has exudative (wet) AMD.1,2 Most likely, if OCT-A had been available during the AREDS study period, subclinical MNV would have been detected more frequently in these dry AMD eyes with the higher risk of progression to exudative disease.
The difference between now and then is that we can easily detect MNV before symptomatic exudation occurs. By knowing that these lesions are present, we might be able to improve our ability to predict when exudation might occur. However, what should we do before this exudation occurs? We just don’t know enough about these asymptomatic lesions to decide if early intervention is a good idea.
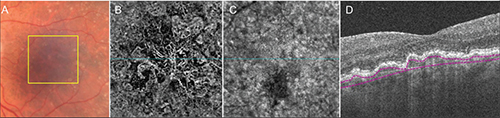 |
| This 81-year-old man has non-exudative age-related macular degeneration in the left eye. A: Color fundus image shows drusen and pigmentary changes in the central macula consistent with non-exudative AMD. The yellow square represents the 3-mm x 3-mm scan area used to create the en face flow image shown in panel B. B: En face OCT-A flow image showing the neovascular complex under the retinal pigment epithelium. C: En face optical coherence tomography angiography structure image corresponds to the en face flow image shown in B. D: Horizontal B-scan corresponding to the blue line in B shows custom segmentation (red lines) under the retinal pigment epithelium used to create the en face flow image in panel B. |
Several recent reports have used OCT-A to document the presence of asymptomatic, subclinical MNV under suspicious drusen and low-lying irregular detachments of the retinal pigment epithelium (Figure).3-5 OCT-A images of these “quiescent” or “subclinical” neovascular lesions confirm what has been known for quite a while. In the 1970s, Richard Green, MD, and Shirley Sarks, MD, detected signs of neovascularization under drusen in histological specimens of eyes with AMD.
In the 1990s, Ferdinando Bottoni, MD, and colleagues and Prut Hanutsaha, MD, and colleagues identified indocyanine green angiography (ICGA) plaques in eyes with dry AMD.8,9 They considered these plaques to be the angiographic feature of subclinical MNV.
In a large series of 432 eyes, ICGA was performed in patients with wet AMD in one eye and dry AMD in their fellow eye, and plaques were detected in 11 percent of eyes with dry AMD.8 The rate of exudative conversion in these eyes with dry AMD varied from 3 to 28 percent per year,8,10,11 but eyes with ICGA plaques were 2.6 times more likely to develop exudative changes within 21 months of follow-up compared with eyes having normal ICGA images. Moreover, these non-exudative lesions tended to enlarge over time, causing visual distortions even in the absence of exudation.12
A New Era in Detection
Even though we’ve known for a while that ICGA could detect eyes at risk for progression to exudation, retina specialists had not routinely performed ICGA for this purpose because of its invasive nature and the risk of an allergic or anaphylactic reaction. Moreover, ICGA is expensive, time-consuming, resource-intensive and uncomfortable for the patient.
Because of these limitations, angiographic monitoring of eyes with intermediate AMD never became routine.
 |
| Dr. Rosenfeld is a professor at Bascom Palmer Eye Institute, University of Miami Miller School of Medicine. He has been the principal investigator and study chair for several clinical trials. Dr. Roisman is post-doctoral associate in retina at Bascom Palmer. |
While we need large studies to better understand the natural history of subclinical MNV, it seems reasonable to assume that these eyes are more likely to progress to active, symptomatic forms of exudative AMD compared with eyes without evidence of MNV.
What Future Studies Can Tell Us
Further study would answer questions like: Should we follow these eyes with asymptomatic MNV more frequently, and if so, how frequently? Should we educate patients differently about their disease? Should we place greater emphasis on home vision monitoring with some of the newer devices that detect visual disturbances? Should these eyes be treated with intravitreal injections of vascular endothelial growth factor (VEGF) inhibitors to prevent growth and exudation? If we do start treatment, then what’s our endpoint for stopping, or how do we decide when to extend the treatment interval? What if anti-VEGF therapy accelerates the formation of macular atrophy by causing regression of the MNV?13 In clinical practice, should we treat these eyes with subclinical MNV any differently than we might treat asymptomatic eyes with early signs of exudation? Do we watch or do we treat?
We can only answer these questions by using OCT-A in large, natural history studies. Now that we have OCT-A, we can no longer ignore non-exudative neovascular intermediate AMD. RS
REFERENCES
1. Mitchell P, Foran S. Age-Related Eye Disease Study severity scale and simplified severity scale for age-related macular degeneration. Arch Ohthalmol. 2005;123:1598-1599.
2. Ferris FL, Davis MD, Clemons TE, et al. A simplified severity scale for age-related macular degeneration: AREDS Report No. 18. Arch Ophthalmol. 2005; 123:1570-4.
3. Palejwala NV, Jia Y, Gao SS, et al. Detection of nonexudative choroidal neovascularization in age-related macular degeneration with optical coherence tomography angiography. Retina. 2015; 35:2204-2211.
4. Querques G, Souied EH. Vascularized drusen: Slowly progressive type 1 neovascularization mimicking drusenoid retinal pigment epithelium elevation. Retina. 2015; 35:2433-2439.
5. Roisman L, Zhang Q, Wang RK, et al. Optical coherence tomography angiography of asymptomatic neovascularization in intermediate age-related macular degeneration. Ophthalmology. 2016. 2016 Feb 12. [Epub ahead of print].
6. Sarks SH. New vessel formation beneath the retinal pigment epithelium in senile eyes. The British journal of ophthalmology. 1973; 57:951-65.
7. Green WR, Key SN 3rd. Senile macular degeneration: a histopathologic study. TTrans Am Ophthalmol Soc. 1977; 75:180-254.
8. Hanutsaha P, Guyer DR, Yannuzzi LA, et al. Indocyanine-green videoangiography of drusen as a possible predictive indicator of exudative maculopathy. Ophthalmology. 1998; 105:1632-1636.
9. Bottoni FG, Aandekerk AL, Deutman AF. Clinical application of digital indocyanine green videoangiography in senile macular degeneration. Graefes Arch Clin Exp Ophthalmol. 1994; 232:458-468.
10. Strahlman ER, Fine SL, Hillis A. The second eye of patients with senile macular degeneration. Archives of ophthalmology. 1983;101:1191-1193.
11. Five-year follow-up of fellow eyes of patients with age-related macular degeneration and unilateral extrafoveal choroidal neovascularization. Macular Photocoagulation Study Group. Arch Ophthalmol. 1993;111:1189-1199.
12. Querques G, Srour M, Massamba N, et al. Functional characterization and multimodal imaging of treatment-naive “quiescent” choroidal neovascularization. Invest Ophthalmol Vis Sci. 2013;54:6886-6892.
13. Grunwald JE, Daniel E, Huang J, et al. Risk of geographic atrophy in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2014;121:150-161.




