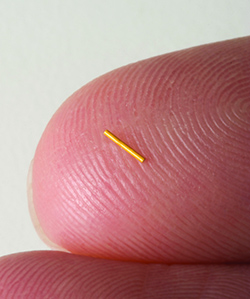
Iluvien releases submicrogram levels of fluocinolone acetonide to the retina for the treatment of DME. The Food and Drug Administration (FDA) approved Iluvien in September 2014, and Alimera
Sciences spent the intervening months building inventory and a sales force, says Dan Myers, Alimera co-founder, president and CEO. Iluvien contains 0.19 mg of fluocinolone acetonide.
When Anti-VEGF Doesn’t Work
Dr. Chen, who practices at Orange County Retina in Southern California and is a member of the Fluocinolone Acetonide in Diabetic Macular Edema (FAME) Study Group, says the implant also meets a need for patients who cannot sustain the burden of monthly anti-VEGF therapy. “Patients with diabetes are usually younger and productive members of society,” Dr. Chen says.“They also frequently have other comorbities (such as heart and kidney disease) that require follow-up at other doctors’ offices. This may make it difficult for them to come into the office every month for intravitreal anti-VEGF injections,” Dr. Chen says.
Another population well-suited to the implant may be non-responders or suboptimal responders to anti- VEGF agents, Dr. Chen says. “We know through research that DME is a multifactorial disease and there is probably more than just a VEGF component; there is likely an inflammatory component to it as well,” he says.
Patients who have had previous vitrectomy or retina surgery represent a lesser-known group that may benefit from the Iluvien implant. “Having the implant may help in their treatment, because once a patient has had a vitrectomy, the anti-VEGF agent literally can be cleared out in a week,” Dr. Chen says. “The pharmacokinetics of the Iluvien implant follows zero-order kinetics and allows for slow release up to 36 months.”
An Education Process
FDA approval of Iluvien culminated a decade-long journey that included three prior negative FDA decisions. The journey started in 2004 when Alimera acquired the rights to the implant for delivering steroids to the back of the eye. At the time, Mr. Myers had recently started Alimera, having previously been with Novartis Ophthalmics, where he served as president from 1997 through 2002.Mr. Myers chalks up the FDA experience as a learning process. “It’s the same learning process about diabetic macular edema that the retina community is going through right now,” he says. The breakthrough was language in the final label indication that required a patient to have had prior steroid treatment with no clinically significant rise in IOP.
“We’ve learned, as the retina specialists have learned, that DME is more of a multifactorial disease than wet age-related macular degeneration,” Mr. Myers says. “Multiple cytokines are involved, and DME has more of an inflammatory aspect than we realized a few years ago.”
In 2011, when the FDA issued a critical Complete Response Letter on Iluvien, clinical opinions about the use of steroids in the treatment of DME were just forming. “Maybe the view questioning if a steroid would be necessary for treating DME in 2011 progressed to where we find ourselves today: where there’s no question there will be a large number of patients who will need both anti-VEGF therapy and treatment by steroids as well,” Mr. Myers says.
Now those patients with DME have a multi-year option. RS




