In the first case, OCT-A helped us to consider a different etiology for a macular hemorrhage
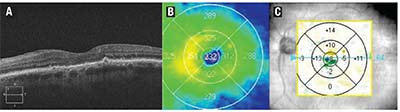 |
| Figure 1. An optical coherence tomography scan OS (A) demonstrates epiretinal membrane and drusen but no intra- or subretinal fluid. Macular thickness map (B) demonstrates normal central retinal thickness (CRT), while retinal change analysis (C) shows no significant change in CRT. |
Case 1: OCT-A Alters Diagnosis
An 87-year-old woman who’s had non-insulin-dependent diabetes for seven years was referred to our clinic in July 2016. She had a history of wet age-related macular degeneration in her right eye, and had been on a treat-and-extend regimen with ranibizumab (Lucentis, Roche/Genentech) since 2013. She had four intravitreal ranibizumab injections in her left eye in 2013-2014 for reasons that were unclear, but most likely due to diabetic macular edema, but had no further injections in the left eye since.
Her visual acuity (VA) was counting fingers (CF) and 20/70 OD and OS, respectively. Geographic atrophy and a macular scar were present in the macula OD, and drusen and a macular scar OS. No signs of diabetic retinopathy were evident in either eye. OCT showed no evidence of intraretinal (IRF) or subretinal (SRF) fluid in either macula. We made the decision to continue intravitreal ranibizumab OD with interval extension to 10 weeks and observation OS.
We saw the patient on two subsequent occasions, extending the interval of ranibizumab to 12 weeks OD and a stable macula OS. On follow-up in March 2017, she reported no visual changes, and her VA was stable at CF and 20/50 OD and OS, respectively.
Examination
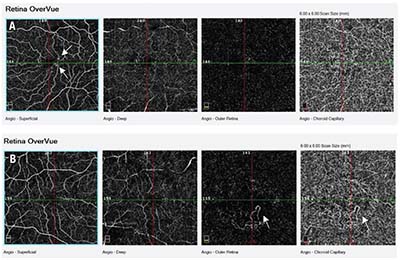 |
| Figure 2. Optical coherence tomography angiography (OCT-A) OS (A) demonstrates no choroidal neovascularization (CNF) in the outer retina/choroid. Dilatation of blood vessels (microaneurysms) appears in the superficial vascular plexus (arrows). OCT-A OD (B) shows quiescent CNV (arrows) in the outer retina and choroid. |
Prior to OCT-A imaging, our presumptive diagnosis was new wet AMD OS. Supporting this were wet AMD in her fellow eye, the clinical appearance of macular drusen, pigmentary changes, hemorrhage and patches of atrophy in the macula OS, and the fact that no diabetic retinopathy had been present in either eye. Main arguments against this diagnosis were stable VA OS, and the lack of SRF/IRF on OCT and OCT-A.
After discussing the clinical and imaging findings with our patient, she consented to an IVFA to clarify the need for anti-VEGF therapy in the left eye. IVFA failed to demonstrate leakage/CNV, supporting the findings on OCT-A (Figure 3). Based on these findings, we chose not to initiate anti-VEGF therapy and instead opted for observation. On her last follow-up in June 2017, she was clinically stable with no sign of wet AMD.
Case 2: Abnormal Flow
This case involves a 55-year-old man with recurrent central serous chorioretinopathy (CSCR) in both eyes, more active in the left. In 2010 he was treated with reduced fluence photodynamic therapy in the left eye, with complete resolution of his SRF. He had recurrence of CSCR in the left eye in 2016 and received thermal laser treatment, with complete resolution of SRF. CSCR recurred in late 2016, which resolved spontaneously. Over time, VA had deteriorated to 20/400 OD due to retinal pigment epithelium atrophy. Vision OS—his good eye—was stable at 20/40.
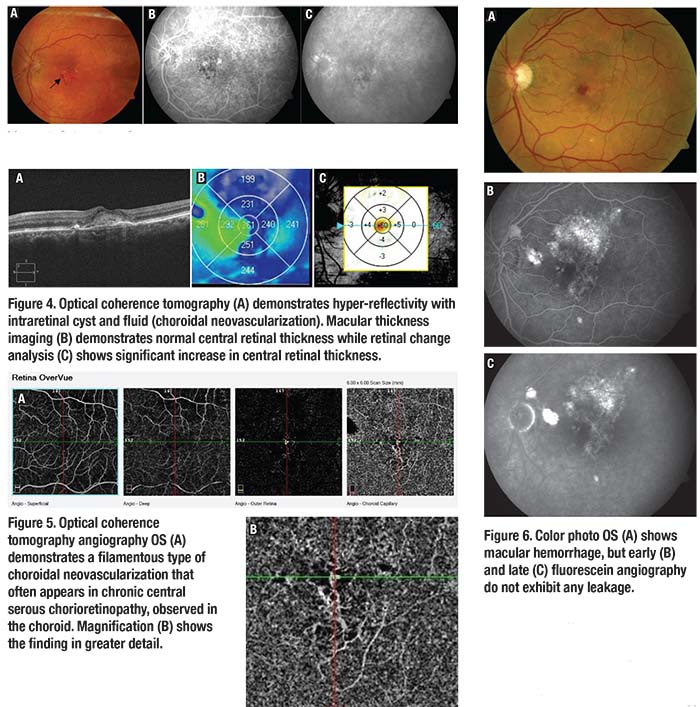 |
He presented to our clinic in March 2017 with a two-week history of decreased vision OS. VA had decreased by two lines to 20/60, and a new macular hemorrhage was present OS. OCT imaging revealed a new hyper-reflective area, with small intraretinal cysts and overlying fluid. The CRT had increased by 60 μm to 261 μm (Figure 4). OCT-A demonstrated flow in the choriocapillaris layer, representing a vascular network. This appeared to be a filamentous-type CNV, often seen in chronic CSCR (Figure 5).
The findings on OCT and OCT-A were consistent with CNV. We completed multimodal imaging by performing an IVFA and, interestingly, found no leakage (CNV) (Figure 6). This patient had a diagnosis of chronic CSCR, with a new macular hemorrhage, intraretinal fluid on OCT, CNV on OCT-A, but no leakage on IVFA.
Our presumptive diagnosis was CNV complicating chronic CSR, and the patient was started on aflibercept (Eylea, Regeneron) OD. After three intravitreal injections, vision improved by 2 lines to 20/50+2, the hemorrhage resolved, and OCT showed no IRF/SRF. At that visit, the patient was treated with his fourth aflibercept injection, and treatment was extended to six weeks.
Dr. Mandelcorn is an assistant professor of ophthalmology at the University of Toronto. Dr. Alon is a retina fellow at the University Health Network (UHN) there. Dr. Brent is a clinician investigator at the Krembil Research Institute at UHN. RS
Disclosures: The authors have no relevant disclosures.




