We all dread a macular hole that didn’t close on the first try. Wider peels, scraping and/or hydrodissecting the edge of the hole, and even radial incisions at the refractory hole have yielded generally unsatisfactory results for this unsatisfying subsequent surgery. More recently, autologous transplantation of internal limiting membrane flaps have come into vogue, but this can be technically challenging and frustrating, as anyone who has tried free- flap transplantation surely knows.
 |
Here, Ferhina Ali, MD, MPH, and Richard Kaiser, MD, from Wills Eye Hospital share a modified approach to ILM flaps in eyes with a previous ILM peel.
A Modified Hinged Flap
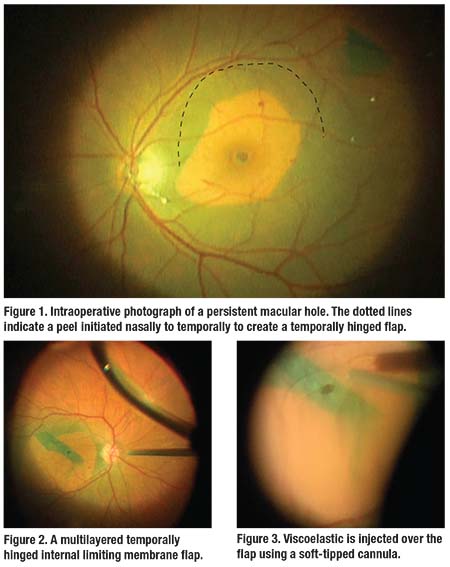
They favor the use of a flap hinged at the edge of the prior peel. They initiate this subsequent peel nasally to create a thin strip of ILM (Figure 1) that is peeled to a temporal hinge, where the strip of peeled ILM is laid over the hole (Figure 2).
A temporal (rather than nasal) hinge helps minimize mispositioning of the flap during air-fluid exchange. If a hinged flap is unobtainable, a free flap from eccentric ILM is then harvested, but this approach can be more technically challenging. The free flap can be difficult to release from the forceps over the hole and to keep in place during air-fluid exchange.
Viscoelastic to Maintain Flap
Drs. Ali and Kaiser inject viscoelastic with a soft-tipped cannula over the flap to tamponade the flap (hinged or free) in position. High magnification allows positioning of the cannula directly over the flap to mitigate the tendency for viscoelastic to disperse throughout the fluid-filled vitreous cavity (Figure 3).
A combination dispersive and cohesive viscoelastic such as Amvisc Plus (Bausch + Lomb) that has high viscosity, high molecular weight, increased surface tension, and adheres well to tissue surfaces is ideal to keep the flap in position. Postoperative intraocular pressure spikes should not occur with this small amount of viscoelastic in the posterior segment.
Air-fluid exchange
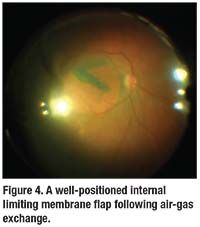
A nasal tilt during air-fluid exchange optimizes positioning of the temporal flap, which will drape over the hole by gravity and with the currents of remaining fluid (Figure 4). Here, longer-acting C3F8 gas may be preferred for tamponade.
 |
This clever modification of the ILM flap maintains a hinge in eyes with a prior ILM peel to reduce the challenges of a free flap. As creative surgeons like Drs. Ali and Kaiser continue to modify the ILM flap, we can hope for a procedure to repair refractory macular holes that is more consistent and approachable than current techniques. RS
Dr. Ali is a vitreoretinal fellow at Wills Eye Hospital, Philadelphia. Dr. Kaiser is a professor of ophthalmology at Thomas Jefferson University and associate surgeon and fellowship codirector at Wills Eye Hospital.




