Restoring useful, functional vision to patients with previously untreatable retinal diseases is a dream that is becoming a reality. Though in its infancy, the use of retinal prostheses to treat patients blinded by outer retinal degenerations is being performed in specialized centers.
At Toronto Western Hospital (TWH), we were the first team in Canada to implant the Argus II Retinal Prosthesis (Second Sight Medical Products) in patients with outer retinal degenerations. Our first patient had surgery in the summer of 2014. Since then we have implanted five additional patients. Here, we share what we’ve learned so far about this device and patient expectations.
What It Is and How It Works
The Argus II is an epiretinal prosthesis designed to electrically stimulate the visual system by bypassing the outer retina. Its goal is to provide these patients with an improvement in their functional vision.
The Argus II system consists of two components: an eyeglass-mounted camera connected to a video processor and battery unit worn on a belt; and an ocular component consisting of a receiving/transmitting coil, electronics case and a 60-electrode array. The array is implanted in an epiretinal location and is secured to the macula using a retinal tack (Figure). It is connected to the electronics housing via a ribbon cable inserted through a 5-mm pars plana incision. The electronics housing is secured to the sclera and is flanked by a receiving coil that sits on a band implanted under the rectus muscles like a scleral buckle.
The camera on the glasses captures an image and sends it to the video processor worn on the belt clip. The processor converts the image into pixels that can stimulate the 60-electrode array. This image is then sent back to the glasses where it is wirelessly transmitted to the receiver coil on the encircling band.
The signal is sent through the electronics housing and down the transmitting coil to the epiretinal array sitting on the macula. The electrodes on the array stimulate the functional inner retina and the signal is sent down the usual visual pathway, thus bypassing the outer retina. The patient perceives an image made up of a combination of 60 phosphenes, or points of light.
The Implant Operation
The surgical steps involved in implantation are familiar to most retinal surgeons. It is similar to performing a scleral buckle, vitrectomy and glaucoma valve.
The surgery begins like any scleral buckling procedure with conjunctival peritomy and isolation of the rectus muscles.
Next, the receiver coil is centered underneath the lateral rectus and the electronics package placed in the superotemporal quadrant and secured with sutures similar to placing a glaucoma valve. The encircling band is placed under the remaining recti and secured with a standard sleeve.
A core and peripheral vitrectomy is performed. A 5-mm pars plana incision is made in the superotemporal quadrant with a microvitreoretinal blade. The precise location of this incision is calculated based on the anatomy and axial length of the eye. The goal is for the array to lie precisely over the macula, with no twisting or tension of the ribbon cable that connects the array to the electronics box.
The array is introduced into the vitreous cavity through the incision. It is tacked to the macula with a retinal tack, which is essentially a sharp miniature tack introduced through the array, retina, choroid and sclera. An engineering team tests the impedance of each electrode intraoperatively. The electronics package and receiver coil are covered by donor pericardium to prevent conjunctival erosion. The eye is closed and the procedure is over.
The Rehabilitation Process
The rehabilitation team begins programming and basic training at postoperative week one. The team creates customized thresholds to ensure that electric current produces a comfortably bright spot of light for the patient. The patient learns basic functions like turning the system on and choosing between different modes. More importantly, the patient learns the minimal skills necessary to enable the system to produce a meaningful image; that is, eye movement and precept localization awareness, eye position and radio frequency link awareness, and head-scanning behavior.
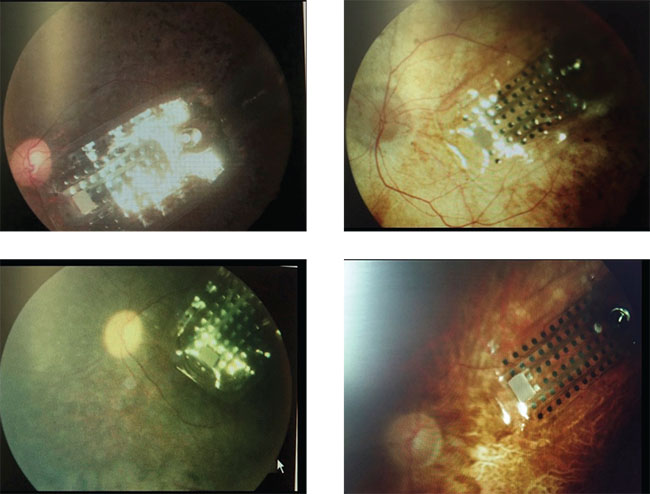 |
| Figure. Fundus photographs showing the array sitting on the macula in four of our first five Argus II patients. |
Following basic training, the patient can begin to start practicing at home. The patient meets with our team to practice and learn the six essential skills: eye, head and camera position awareness and movement; small-scale light localization (microscanning); large-scale light localization (macroscanning); tracking; luminance discrimination; and shape recognition.
The most important part of visual rehabilitation is setting realistic goals. The Argus II is a low-vision device, a 10-by-6 array that can provide a 20-degree field of vision. Patients who expect the device to restore “normal vision” will always be disappointed. Argus II is unlike any other low-vision tool in that it can improve activities of daily living and assist in orientation and mobility. Selecting patients who understand that, and setting appropriate goals before and after surgery, are keys to a successful outcome.
The Canadian Perspective
To our knowledge, TWH is the only site in Canada with experience in providing the Argus II to multiple patients. Our team consists of the surgeon, fellows and residents, surgical nurses, rehabilitation ophthalmologists and optometrists, surgical coordinators, engineers from Second Sight, our hospital foundation and the families of patients. We have funding to provide a total of 10 Argus II devices from a donor through our hospital foundation.
The price of the implant alone is more than $107,000 U.S. and $140,000 Canadian. We hope that one day our provincial health-care system will cover it. We screen patients from all over Canada who are 25 years old and older, have severe to profound retinitis pigmentosa, bare light perception or no light perception with a functional inner retina, and have a history of prior useful form vision.
Variable Patient Results
Our results have been variable. Some patients describe it as a life-changing experience and even, remarkably, say they are able to read some letters on the eye chart. Others no longer use the device. Our younger patients seem to be doing better with the new technology. Approximately one-third of our patients are very happy, one-third somewhat happy and one-third less so. We are getting better at predicting who will do well with this technology and we hope to have even happier patients as our understanding of patient selection improves.
There is certainly a learning curve with any new, state-of-the art technology. We have found the Argus II to be a challenging, exciting and worthwhile experience. The idea of giving useful vision back to someone with no-light-perception vision seems like science fiction, but it is happening in Toronto. We are grateful to be involved and excited to see what we can achieve for patients that we, as vitreoretinal surgeons, once had nothing to offer. RS
The authors are with the University of Toronto Department of Ophthalmology and Vision Sciences, University Health Network/Toronto Western Hospital Department of Ophthalmology.



