|
• Which agent do we use?
• How often do we give it?
• If and when should we stop treatment?
Multiple randomized, controlled clinical trials have demonstrated the short-term efficacy and safety of these agents. However, there has been a dearth of long-term data to guide us in our chronic management or to provide us long-term treatment expectations for our patients. Here, we try to answer those questions.
The Early Trials
Nearly 10 years ago, the two landmark ANCHOR and MARINA trials demonstrated the efficacy and safety of monthly ranibizumab (Lucentis, Genentech) over the course of two years. Patients gained 10.7 and 6.6 letters, respectively, at two years.1-3
Five years later, the parallel studies, VIEW1 and VIEW2, similarly showed improvement in vision with aflibercept administered every eight weeks after three initial monthly loading doses at the studies’ one- and two-year endpoints.4 Subsequent randomized multicenter trials have allowed us to evaluate the efficacy of these drugs compared to off-label bevacizumab (Avastin, Genentech), as well as to investigate other less-frequent dosing intervals, including quarterly and PRN regimens.
While each of these treatment strategies has shown benefit over observation, the visual acuity outcomes are inferior compared to monthly treatment. The PIER study examined quarterly dosing after three monthly loading doses, and, while superior to observation, PIER patients lost 2.3 letters from baseline at one year.5 EXCITE compared quarterly dosing to monthly therapy and, once again, while the quarterly arms did not reach pre-specified non-inferiority compared to the monthly arm at one year, the results were clearly better with more frequent dosing.6
One of the earliest exceptions was PrONTO, a Phase I/II trial that involved 40 patients over two years on a monthly PRN basis using visual acuity, clinical examination and optical coherence tomography parameters as guidelines for re-treatment.7 The visual acuity results approached those of ANCHOR and MARINA with nearly half the number of injections, but the study lacked a monthly-treatment control arm.
CATT and HARBOR had monthly and PRN treatment arms. While these studies demonstrated statistically similar results with monthly dosing in the short term, absolute data outcomes were almost unanimously superior with monthly dosing. What’s more, long-term outcomes may reveal inferiority of alternative treatment strategies as the two-year results of the bevacizumab PRN group in the CATT trial showed.8
While the aforementioned studies have been crucial in guiding our management and treatment of exudative AMD, the treatment protocols can be onerous to adhere to in clinical practice. Many retinal physicians gravitate toward less-frequent examination and dosing regimens. Frank Holz, MD, and colleagues demonstrated that this has resulted in poorer visual outcomes in “real-world” clinical scenarios compared to published study results (Figure 1).9
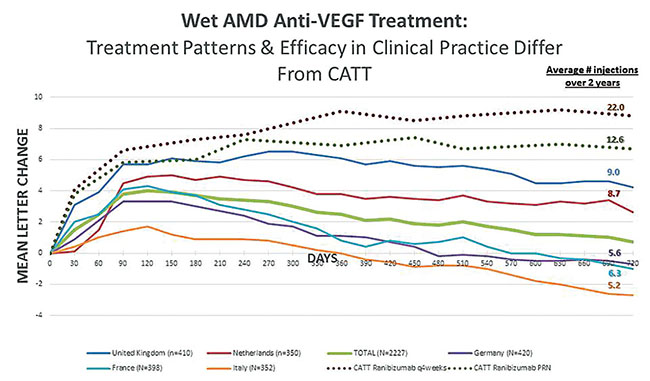 |
| Figure 1. Under-treatment of wet AMD in clinical practice leads to visual outcomes worse than those seen in controlled clinical trials. In the studies cited here, decrease in mean visual acuity from baseline correlated to fewer injections. |
Treat-and-extend regimens, as Michael Englebert, MD, PhD, and colleagues initially described them, however, offer a hybrid option that allows continuous dosing with less rigorous monitoring than PrONTO protocols, while resulting in fewer injections and visual outcomes similar to monthly dosing, at least in the short term.10
A recent retrospective study examining three-year outcomes reported visual gains comparable to other studies where patients received monthly therapy with an average of 6.4 yearly injections over three years.10 While all of these studies offer guidance with regards to efficacy of various drugs and treatment intervals, they are limited to short follow-up (one to three years); thus they fail to address outcomes over prolonged treatment.
Unfortunately, due to a lack of long-term outcomes data, physicians have been relegated to extrapolating this short-term data into the chronic management of wet AMD.
Long-Term Data, Such as It Is
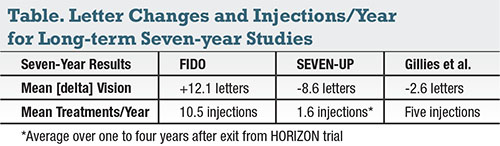
CATT showed that visual gains of PRN dosing with bevacizumab were inferior to those with monthly ranibizumab after the first year. These discrepancies over time raised the question of whether additional temporal divergences might occur over the long term. Given the expense of large, randomized trials, treatment data has essentially been limited to two-year outcomes with a few exceptions mentioned herein. Only recently, with data from HORIZON, SEVEN-UP, FIDO, CATT and the observational study by Mark Gillies, MD, and colleagues, have we seen that a divergence in visual acuity outcomes between the various treatment regimens does indeed play out with time (Figure 2, Table).11-15
 |
The HORIZON extension trial followed patients exiting from the ANCHOR and MARINA trials after two years of monthly therapy.11 These patients then had treatment and monitoring on average every two months PRN. Within one year, the impressive 9-letter gain initially reported with monthly therapy dropped to 4.1 letters. Visual loss continued over the ensuing two years, with patients demonstrating a mean 0.1-letter loss from baseline.
An additional cohort from HORIZON was further evaluated in the SEVEN-UP study that added three years of follow-up of patients exiting HORIZON after four years of therapy.12 They experienced further vision loss, ending up 8.6 letters below baseline (Figure 2). However, eyes only received an average of 6.8 injections over the 3.4 years after exit from HORIZON. Most notably, approximately 41 percent of eyes received no treatment at all.
A separate univariate analysis found that patients receiving 11 or more injections after exit from HORIZON actually gained 3.9 letters, ending up 5.6 letters better than baseline after seven years (Figure 3). It is important to note that PRN protocols seen in HORIZON/SEVEN-UP differed from standard PrONTO-based monitoring and retreatment criteria, which specify monthly monitoring. More stringent PRN protocols with prescribed OCT-guided retreatment may result in outcomes superior to these reported PRN results. However, once again, the long-term data is lacking.
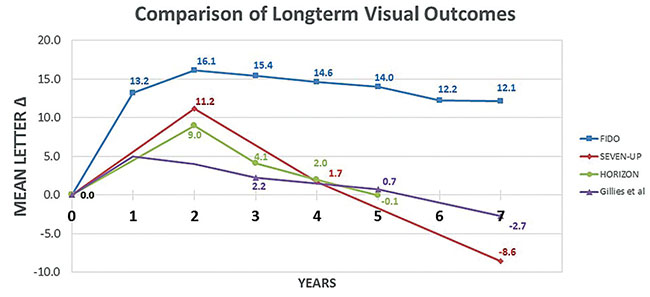 |
| Figure 2. Long-term mean letter change over time in patients receiving anti-VEGF therapy for wet age-related macular degeneration. |
Last year, an observational study reporting seven-year outcomes of treatment-naïve patients receiving anti-VEGF therapy at the discretion of 23 different specialists demonstrated slightly better results with a greater average number of injections.14 Of the 131 eyes with the longest follow-up, a 2.7-letter loss from baseline was noted at seven years (Figure 2), with 40 percent of patients maintaining 20/40 vision compared to 32 percent at baseline.
Eyes received six injections on average in the first year, five injections between years two and five, and 5.5 injections in years six and seven. While this study did not report a percentage breakdown of the various treatment regimens, the authors did state that the majority of investigators favored a treat-and-extend approach—consistent with a higher average number of injections than the SEVEN-UP study. More injections, however, were also associated with improved visual outcomes when compared to SEVEN-UP.
The CATT trial most recently released its five-year data. The results were equally disappointing as the results seen in Dr. Gillies’ observational studies, as patients lost a mean 3 letters compared to baseline and 11 letters from the two-year CATT outcomes.15 After completing two years of the CATT protocol, patients were no longer evaluated and treated according to protocol, and physicians treated them according to their normal practice patterns with regard to frequency and agent.
Over the ensuing three years, there was a bias toward bevacizumab along with decreased frequency of treatment. Of the patients originally in the ranibizumab arms, 53 percent were treated with bevacizumab or bevacizumab in combination with ranibizumab and/or aflibercept (Eylea, Regeneron Pharmaceuticals). In the original bevacizumab arms, 62 percent were continued on bevacizumab alone or in conjunction with ranibizumab and/or aflibercept.
Furthermore, patients originally in the ranibizumab monthly and PRN arms received 10.7 and 5.7 injections in the second year of CATT, respectively, while those in the bevacizumab monthly and PRN arms received 11.5 and 6.8 injections in the second year, respectively.8 Over the next three years, the combined cohort received an average of 4.8, 4.5 and 4.0 injections in the third, fourth and fifth years, respectively.
At five years, this difference amounted to as much as a 65-percent reduction in treatment frequency for those eyes in the bevacizumab monthly arm and 31-to-41-percent reduction in the eyes originally assigned to ranibizumab and bevacizumab PRN arms, respectively. The drop in vision in conjunction with increased bevacizumab use on a less-frequent dosing regimen would confer greater evidence as to the inferiority seen at two years in the bevacizumab PRN arm compared to monthly ranibizumab.
In our FIDO study published last year, patients achieved visual acuity gains with continuous dosing over seven years.13 In this retrospective study, we identified 44 eyes with at least seven years of consistent treatment with continuous, fixed-interval dosing between four and eight weeks. This provided a unique data set to explore the effect of prolonged continuous exposure to anti-VEGF therapy in wet AMD.
Similar to the previously mentioned studies, our cohort demonstrated significant visual gains that peaked at year two (+16.1 letters). Between years two and seven, a trend toward a 0.8-letter/year decline emerged, with an overall 12.1-letter gain from baseline at seven years (Figure 2). The percentage of patients maintaining driving vision at seven years was comparable to Dr. Gillies’ study at 43.2 percent compared to the 23 percent SEVEN-UP reported.12,14
So Why Fewer Injections?
 |
| Figure 3. This bar graph shows mean letter change based upon number of injections received after exiting HORIZON. Patients in the highest quartile (11 or more injections) maintained visual acuity better than baseline. |
The basic tenet of continuous, fixed-interval dosing is to maintain therapeutic levels of VEGF suppression to prevent new vessel formation, leakage, bleeding and fibrosis. The three studies with seven-year data demonstrated a direct correlation between number of injections and visual acuities (Table). So if short-term and long-term data point toward improved outcomes with more rigorous injection schedules, then why is there a trend toward fewer injections?
The answer is complex and multifactorial, but one can certainly cite the burden of frequent visits and treatment to practices, patients and families. In fact, the most recent American Society of Retina Specialists preferences and trends (PAT) survey found that 47 percent of physicians felt it was due to both them and patients preferring less-frequent dosing even at the risk of decreased visual acuity.16
Perhaps more importantly, we must acknowledge that these injections come with a cost and an inherent risk to the patient when we consider complications such as endophthalmitis and retinal detachment. But are there other risks that treating physicians are worried about?
While VEGF can lead to the deleterious effects seen with choroidal neovascular complex formation, it is neurotrophic for retinal photoreceptors and retinal pigment epithelium cells. Indeed, VEGF-A knock-out mice demonstrated progressive atrophy of the choriocapillaris with ensuing photoreceptor dysfunction and loss.17 Subanalyses from CATT reported a 1.59 greater risk of geographic atrophy (GA) in eyes receiving monthly therapy compared to PRN.8 Other studies have confirmed atrophy, with 89.7 percent demonstrating central atrophy in SEVEN-UP, but Dr. Gillies’ study attributed only 37 percent of vision loss to central atrophy.12,14
Despite the increased prevalence of atrophy in patients receiving more sustained VEGF suppression, we cannot infer a direct causation. A recent study by Miho Tanaka, MD, and colleagues demonstrated that after 3.5 years, GA did not tend to occur outside the boundaries of the initial choroidal neovascularization (CNV) unless the eyes had GA outside this area at baseline.18 Subsequent analysis of the CATT study data also seemed to refute a direct causation between increased VEGF suppression and GA.
Despite the increased prevalence of GA reported in the initial study, the rates of growth were nearly identical at 0.43 mm per year and 0.44 mm per year in the PRN and monthly groups, respectively.19 Giovanni Staurenghi, MD, performed another analysis of the data that pointed toward the increased prevalence of patients with reticular pseudodrusen and retinal angiomatous proliferation in the subgroups that had a higher incidence of GA.20 These particular wet AMD phenotypes have been associated with higher risk toward development of GA and may have affected the original conclusions as well.
 |
The GA controversy is certainly not over. The ASRS PAT survey reported that 31 percent retina specialists still believe that anti-VEGF causes macular atrophy and an additional 40 percent are unsure of the relationship.16
A recent publication may help alleviate some of this concern. The SEVEN-UP fellow-eye study looked at prevalence and growth of GA in both study eyes and fellow eyes.21 Patients initially enrolled in the ANCHOR and MARINA trials were ineligible for treatment in the fellow eye, allowing for a natural progression comparison. After seven years, macular atrophy progression was more severe in the fellow eyes that were exudative at baseline, while fellow eyes that remained non-exudative showed the least amount of atrophy.
Comparisons between eyes of individual patients demonstrated a mean change in area of 4.1 mm2 in those fellow eyes that were exudative at baseline and left untreated for two years, while the study eyes showed a mean increase of only 2.2 mm2. These findings give credence to the hypothesis that continuous exposure of photoreceptors and RPE cells to subretinal fluid, intraretinal fluid and blood may accelerate the progression of atrophy, contradicting concerns of the two-year CATT data and suggesting that continuous anti-VEGF treatment may actually be protective and reduce the rate of progression of macular atrophy in the long term.
Where Do We Go From Here?
While available long-term data is limited in that it is retrospective, the preponderance of evidence points toward improved outcomes with sustained exposure to anti-VEGF agents in patients with wet AMD. With new data suggesting that such therapy may actually delay the progression of GA, the groundwork for the benefit of sustained-release delivery of these agents has been laid.
How we will use these agents with novel pharmacologics is an exciting prospect for retina specialists and our patients. Perhaps by limiting fibrosis with anti-platelet derived growth factor agents, we may also observe a delay in the progression of atrophy. What’s more, while atrophy seems to be an inevitable process in both exudative and non-exudative AMD, perhaps combined therapy with complement inhibitors will further reduce progression. Only the future will tell, but in the meantime, treat early and often with VEGF inhibitors. RS
REFERENCES
1. Brown DM, Kaiser PK, Michels M, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1432-1444.
2. Rosenfeld PJ, Brown DM, Heier JS, et al. MARINA Study Group. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1419-1431.
3. Brown DM, Michels M, Kaiser PK, et al. Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: Two-year results of the ANCHOR study. Ophthalmology. 2009;116:57-65.
4. Schmidt-Erfurth U, Kaiser PK, Korobelnik JF, et al. Intravitreal aflibercept injection for neovascular age-related macular degeneration: ninety-six-week results of the VIEW studies. Ophthalmology. 2014;121:193-201.
5. Regillo CD, Brown DM, Abraham P, et al. Randomized, double-masked, sham-controlled trial of ranibizumab for neovascular age-related macular degeneration: PIER Study year 1. Am J Ophthalmol. 2008;145:239-248.
6. Schmidt-Erfurth U, Eldem B, Guymer R, et al. Efficacy and safety of monthly versus quarterly ranibizumab treatment in neovascular age-related macular degeneration: the EXCITE study. Ophthalmology. 2011;118:831-839.
7. Lalwani GA, Rosenfeld PJ, Fung AE, et al. A variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: year 2 of the PrONTO Study. Am J Ophthalmol. 2009;148:43-58.
8. Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group, Martin DF, Maguire MG, Fine SL, et al. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology. 2012;119:1388-1398.
9. Holz FG, Tadayoni R, Beatty S, et al. Multi-country real-life experience of anti-vascular endothelial growth factor therapy for wet age-related macular degeneration. Br J Ophthalmol. 2015;99:220-226.
10. Engelbert M, Zweifel SA, Freund KB. “Treat and extend” dosing of intravitreal anti-vascular endothelial growth factor therapy for type 3 neovascularization/retinal angiomatous proliferation. Retina. 2009;29:1424-1431.
11. Singer MA, Awh CC, Sadda S, et al. HORIZON: An open-label extension trial of ranibizumab for choroidal neovascularization secondary to age-related macular degeneration. Ophthalmology. 2012;119:1175-1183.
12. Rofagha S, Bhisitkul RB, Boyer DS, et al. Seven-year outcomes in ranibizumab-treated patients in ANCHOR, MARINA, and HORIZON: a multicenter cohort study (SEVEN-UP). Ophthalmology. 2013;120:2292-2299.
13. Peden MC, Suñer IJ, Hammer ME, Grizzard WS. Long-term outcomes in eyes receiving fixed-interval dosing of anti-vascular endothelial growth factor agents for wet age-related macular degeneration. Ophthalmology. 2015;122:803-808.
14. Gillies MC, Campain A, Barthelmes D, et al. Long-term outcomes of treatment of neovascular age-related macular degeneration: data from an observational study. Ophthalmology. 2015;122:1837-1845.
15. Maguire MG, Martin DF, Ying GS, et al. Five-year outcomes with anti-vascular endothelial growth factor treatment of neovascular age-related macular degeneration: the Comparison of Age-Related Macular Degeneration Treatments Trials. Ophthalmology. April 20, 2016. [Epub ahead of print]
16. Stone TW, ed. ASRS 2016 Preferences and Trends Membership Survey (preliminary data). Chicago, IL. American Society of Retina Specialists. Available at: https://www.asrs.org/asrs-community/pat-survey. Accessed May 17, 2016.
17. Kurihara T, Westneskow PD, Bravo S, et al. Targeted deletion of VEGF-A in adult mice induces vision loss. J Clin Invest Ophthalmol. 2012:122;4213-4217.
18. Tanaka E, Chaikitmongkol V, Bressler SB, Bressler NM. Vision-threatening lesions developing with longer-term follow-up after treatment of neovascular age-related macular degeneration. Ophthalmology. 2015;122:153-161.
19. Grunwald JE, Pistilli M, Ying GS, et al. Growth of geographic atrophy in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2015;122:809-816.
20. Staurenghi G. Macular atrophy in anti-VEGF treatment. Paper presented at 44th Annual Aspen Retinal Detachment Society Meeting; March 5–9, 2016;Aspen, CO.
21. Bhisitkul RB, Desai SJ, Boyer DS, et al. Fellow Eye Comparisons for 7-Year Outcomes in Ranibizumab-treated AMD Subjects from ANCHOR, MARINA, and HORIZON (SEVEN-UP Study). Ophthalmology. March 17, 2016. [Epub ahead of print].